OUR LIPOLEXICON
Lipedema:
Everything you need to know
This page provides comprehensive information about lipedema to ensure you are well-informed. Our goal is to empower you to become an expert on your condition and be well-prepared for surgery. We are committed to raising awareness and providing more information about lipedema, and as an affected individual, you can actively contribute to this effort.
Become an ambassador for lipedema and share your knowledge and experiences to help others affected by the condition. Together, we can remove the stigma surrounding lipedema and foster greater understanding and acceptance in society.
What is lipedema?
Lipedema is an extremely debilitating condition resulting from a pathological fat distribution disorder, causing pressure pain and feelings of tightness in those affected. Unfortunately, it primarily affects women, who may have to suffer from the symptoms for years. Lipedema is classified into three different stages and four different types to allow for appropriate treatment.
Causes of lipedema
The causes of lipedema are complex and not yet fully understood. Currently, however, doctors and researchers assume that in approximately 85% of all cases it is triggered by hormonal changes, such as those that occur during puberty or pregnancy. The female hormone estrogen plays a key role here, as it leads to the proliferation and enlargement of fat cells. In addition, a hereditary predisposition plays a role, representing another possible cause.
Onset of lipedema
The occurrence of lipedema is extremely unfortunate, as it is a condition that affects only specific parts of the body. Scientific evidence has so far only been established for the legs and arms, while it has not yet been proven to occur in other areas. The thighs of patients are particularly affected, being the most severely impacted in 97% of cases. However, lipedema can also occur in the buttocks and hips, which makes the condition even more distressing. It has also been shown that typical signs of lipedema can be observed in the arms of patients in 31% of cases. This condition is extremely burdensome and can lead to significant physical and psychological distress for those affected. However, our experienced surgeons have specialized in the treatment of lipedema and are able to recognize the precursors of lipedema, even in the asymptomatic stage, which will later develop into a condition requiring surgery. In this way, we can intervene early and offer our patients successful and sustainable therapy that improves their quality of life.
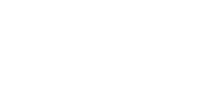
Lipedema symptoms
The diagnosis of lipedema presents a significant challenge for many affected women, as the symptoms are often difficult to classify due to their nature and similarity to other conditions. Diseases such as restless legs syndrome, polyneuropathy, and chronic venous insufficiency exhibit similar symptoms to lipedema. These include pain and feelings of tightness in the legs, as well as abnormal sensations in the arms and legs. Exhaustion and fatigue can also occur in all of these conditions, further complicating diagnosis.
To differentiate lipedema from other diseases, the symptoms are divided into primary and secondary symptoms. Primary symptoms are defined as particularly noticeable and primarily perceived symptoms that are crucial for diagnosing and differentiating lipedema from the aforementioned diseases.
The main symptoms of lipedema include, among others:
- Body proportions that are disproportionate to the rest of the body (e.g., thick legs with a slim upper body)
- Tendency to bruise easily
- Pain and tightness in the legs and arms
- Orange peel skin and cellulite
- Affected body areas feel cold
- Pain cannot be relieved by physical activity or elevating the legs
- Symmetrical distribution of fat deposits on the legs and/or arms
- Due to the difficulty of self-diagnosis of these symptoms, it is important that affected women consult a specialist for diagnosis. Please feel free to schedule an appointment for our diagnostic consultation.
Lipedema stages and types

To further differentiate the severity of lipedema, there are four different types:
Type 1: Lipedema in the legs, no or only minor effects on the arms
Type 2: Lipedema in the legs with effects on the arms
Type 3: Lipedema affecting the legs and arms, with partial involvement of the trunk
Type 4: Lipedema affecting the legs and arms, with complete involvement of the trunk
The classification into stages and types helps to find the appropriate therapy for patients and to monitor the course of the disease. Early diagnosis and treatment can help to avoid complications such as inflammation or thrombosis.
Lipedema surgery
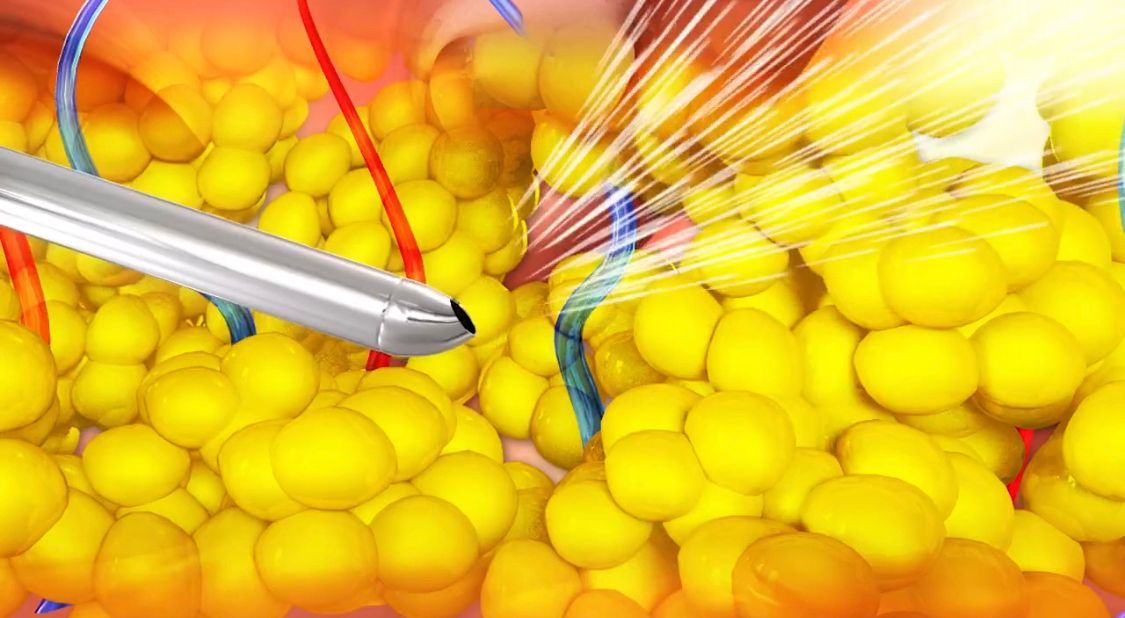
To treat lipedema effectively, liposuction is performed as part of lipedema surgery. With competent and consistent execution of the procedure, excellent results with very few complications can be expected.
Before the operation, it is of utmost importance that patients wear flat-knit compression stockings continuously for six to eight weeks to decongest the tissue and optimally prepare it for liposuction. If the tissue is severely congested, targeted manual lymphatic drainage is also necessary before the operation. This is part of the post-operative care to further decongest and massage the tissue to prevent lymphatic congestion. The flat-knit compression stockings are not only part of the preparation for the operation but also part of the best possible aftercare. The flat-knit compression protects the tissue and prevents hardening, which in turn benefits the skin's retraction.
The day of surgery at the LipoCenter

To give you and your family an idea of what the day of your operation at the LipoZentrum Dr. Heck might be like, we have outlined a sample daily schedule below: (Please note that your personal stay may, of course, differ slightly from what is described.)
You will arrive at the LipoCenter on an empty stomach at your personal check-in time, which will be communicated to you by our staff. You will fill out your documents and be taken to the changing room. There you will put on the surgical gown, remove your jewelry, and have the surgical cap placed on your head.
This is followed by a pre-anesthesia consultation, which is tailored to your individual needs and conducted in detail by the anesthesiologist. The anesthesiologist will insert an intravenous line through which you will receive medication during the operation.
Once all the formalities are completed, our nurses will collect you, and you can decide whether you would like to take your mobile phone into the operating room. Since lipedema liposuction is an exciting and long-awaited moment for many patients, many women want to capture this moment with a photograph. Our nurses and caregivers will gladly do this for you.
Once you arrive in the operating room, you will be weighed and scrubbed to disinfect the surgical area. You will then be placed on the operating table and draped. The anesthesiologist will administer the medication, and you will drift off to sleep. Of course, you can also opt for general anesthesia. After the operation is successfully completed, the nurses will help you put on your surgical gown while you are still on the operating table and take you to the recovery room, where a pre-warmed bed awaits you.
Once you have recovered sufficiently, a nurse will take you to your room and you will enjoy a delicious dinner with your fellow lipedema patients of the day!
Time after surgery
Once you have taken the first step into a new life and successfully completed the operations at the LipoCenter, you should keep a few things in mind:
In the first weeks and months after surgery, the healing and remodeling processes in the operated areas can be most intense, which can lead to tingling, hardening, and swelling. The healing process can take up to a year—in some cases even longer. Your lymphatic system, nervous system, and all the tissue in the surgical area are regenerating, and this takes time and is noticeable during this period.
Give your body time and rest, and remember that liposuction for lipedema is not a minor procedure. If you have any concerns or questions, please feel free to contact us at the LipoCenter; we are here to help.
Lipedema and nutrition

The relationship between a ketogenic diet and lipedema is often discussed. But why is that?
Why should patients with lipedema generally avoid sugar?
Sugar promotes swelling, weight gain, inflammation, and pain. Excessive sugar consumption can also increase the risk of diabetes. Many nutritionists therefore recommend a balanced diet with whole grains. However, the problem is that these foods also contain carbohydrates and therefore sugar. When sugar from food enters the bloodstream, the pancreas produces insulin, which transports the sugar into the cells. If insulin levels remain too high, insulin resistance can develop, which can be a first step towards diabetes. This disease can lead to calcification and deposits in the blood vessels, causing strokes, heart attacks, and high blood pressure.
A ketogenic diet can help reduce hunger and thus sugar intake. However, if you're following a ketogenic diet alone, those who eat carbohydrates may quickly become hungry again. Therefore, try to motivate your partner to also largely eliminate carbohydrates from their diet. Changing your eating habits can help you stay healthy, avoid constant hunger, and achieve a better physique without having to exercise a lot.
Lipedema in numbers – a scientific perspective
Numbers that count – all about lipedema
8%
of body weight may be removed during the operation.
11%
Lipedema affects women worldwide.
80%
Those affected also have lipedema fat in their arms.
1940
Lipedema was first mentioned as a disease by researchers Allen and Hines.
FAQs
Frequently asked questions about lipedema from our patients. We are always here for you and want to ensure you have all the latest information. Therefore, we have answered frequently asked questions about treatment, as well as general questions about your surgery. This information is continuously updated.
Can lipedema recur in other areas?
Lipedema has so far only been scientifically proven in the arms and legs. After surgery, you must ensure you exercise regularly and eat a healthy diet. The lipedema will not recur in the treated areas, but you will naturally gain weight if you consume a calorie surplus. However, this will not be the painful lipedema fat.
Is there always pain with lipedema?
Yes, but pain is subjective. Lipedema often begins gradually during puberty. Many women suffer from lipedema for years, and the pain or heaviness becomes part of their reality. Their legs feel heavy, and pressure causes pain. Their legs are tired after a long day, and climbing stairs becomes difficult.
Is it possible to have the entire legs done in one operation?
Unfortunately, that's not possible. We're only allowed to remove up to 8% of your body weight per surgery. This would create a very large wound area, and anything more would be too much for your body. Most patients need two to three surgeries on their legs. It depends on the volume of tissue.
How can I find out if I have lipedema?
You are welcome to use our diagnostic consultation service or to consult a phlebologist in your area. The diagnosis can also generally be made by general practitioners or gynecologists. Unfortunately, many patients are not taken seriously with their complaints or receive incorrect advice.
Will the health insurance cover the costs?
Unfortunately, health insurance very rarely covers the costs, and then only in stage 3 cases with a BMI under 35. However, we are a private clinic, and you will then be referred to a contracted hospital. All our patients are self-paying.
Should I have the surgery before or after pregnancy?
We advise our patients to have the surgeries done before a planned pregnancy, if possible. This way, you are already rid of the painful lipedema and don't have to deal with additional discomfort or a possible worsening of symptoms during pregnancy.
What is the best diet for lipedema?
We recommend that our patients drastically reduce their carbohydrate intake and largely eliminate sugar. Sugar can lead to micro-inflammation and thus further intensify lipedema pain. However, the right diet is individual – it is important that you eat a balanced diet and do not try to put additional strain on yourself by starving yourself before surgery. A weakened body will recover less well after the procedure.
How long does pain last after surgery?
After the operation, you will need patience. Your legs will be severely swollen for about two to three weeks. Movement while wearing compression garments promotes healing and supports lymphatic drainage. Regular manual lymphatic drainage is helpful. Ibuprofen can also help relieve pain, but this should be discussed with your doctor beforehand. Over time, the symptoms will improve significantly.
When can I go swimming again after the surgery?
Swimming can significantly accelerate the healing process after surgery, as it promotes lymphatic drainage and gently supports the muscles. However, please wait until the stitches have been removed before swimming again.
When can I go back into the sun after the surgery?
Please wait until after the healing year. If you tan beforehand, the scars may become permanently darker.
When can I shower again after the surgery?
Take a shower on the second day after your surgery. Please do not shower alone, as this can cause circulatory problems. It's best to remove your compression garment while sitting in the shower and take the opportunity to wash it thoroughly.
How long do I need to wear the compression garment?
As preparation for the surgery, you must wear the compression garment consistently. The duration will be determined during your consultation. After the surgery, you will wear the compression garment day and night for six weeks, and then during the day for two weeks.
When will I be discharged after my surgery?
You will spend one night in the clinic and will be discharged the following morning between 7:00 and 7:30 a.m. Please arrange for someone to pick you up and help you get home.
Will I receive general anesthesia?
Whether you will receive general anesthesia can be discussed with your anesthesiologist, and you are free to decide. Alternatively, you can also choose twilight sedation.
By when does the clinic need the blood test results?
We need your blood test 10-14 days before the operation (see checklist).
What must be shown in the blood test?
We need a complete blood count including Hb value as well as the coagulation values INR, PTT and Quick.
How old can the blood test be?
The blood test must not be older than 14 days.
How much does liposuction for lipedema cost?
The surgery for lipedema costs €7,480 at our clinic, regardless of the surgical area.